Sacroiliac Joint Fusion
The sacrum is the lower portion of the spine where several vertebrae are fused together. The sacrum is a triangular shaped bone that has a joint on either side with the ilium, the back part of the pelvis. The pubic rami, the front part of the pelvis, fit together in the front forming the pubic symphysis. The sacroiliac joints are L shaped in contour with a shorter upper and longer lower arm. Normally the sacroiliac joint is configured in such a way that the bones have an interlocking structure, which assists in keeping them properly aligned. In some cases the opposing joint surfaces are quite flat. This type of joint is much less stable and can lead to a shearing or sliding malalignment. Some sacroiliac joints reverse the normal concave-convex ‘locking’ relationship, which can lead to rotational malalignment. The variation in joint configuration results in a corresponding variation in integrity. This means that some people are more susceptible to SI joint pain because the joints are inherently weaker or more prone to malalignment.
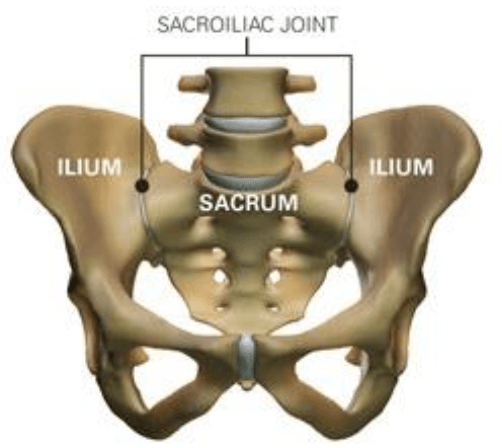
Figure 1. (Top view of the Sacrum and where Sacroiliac Join Pain reflects)
Request An Appointment
Who is a candidate?
There are several different factors that can cause SI joint pain and dysfunction. One of the most common causes is an injury. The injury can come from a direct fall on the buttocks, a motor vehicle accident or a sports related trauma. The force from these injuries can strain the ligaments around the joint. Tearing of these ligaments can lead to hypermobility in the joint. This excess motion and lack of stability is thought to be the main cause behind sacroiliac joint dysfunction. Pregnancy may also be a factor in the development of SI joint pain. Women secrete the ‘relaxin’ hormone during pregnancy. This hormone allows the connective tissues in the body to relax. The relaxation is needed so the pelvis can stretch enough to allow the baby to pass during labor. This stretching may affect the SI joints causing them to become hypermobile. The more pregnancies a woman has, the more chance she has of developing SI joint pain.
Leg length discrepancies may also play a role in sacroiliac joint dysfunction. If a person has one leg that is shorter than the other, the abnormal alignment may end up causing SI joint pain or malalignment issues.
Often, an exact cause leading to SI joint pain cannot be found. The joint simply becomes painful, and the patient and their local physician do not have an answer as to why the joint has become troublesome. It takes a trained health care provider to accurately diagnose and treat sacroiliac joint pain.
Common Symptoms:
Common symptoms of sacroiliac joint dysfunction:
- Lumbosacral pain
- Buttock Pain
- Pain radiating to the leg
- Hip pain
- Groin pain
- Urinary frequency
- Iliac crest pain
- Transient numbness, prickling or tingling
- Increased pain with menstruation
- Increased pain with sexual intercourse
- Increased pain with stair climbing
- Increased pain with sustained positions (i.e., sitting, walking, lying)
What happens before surgery?
You may be scheduled for presurgical tests (e.g., blood test, electrocardiogram, chest X-ray) several days before surgery. In the doctor’s office, you will sign consent and other forms so that the surgeon knows your medical history (allergies, medicines/vitamins, bleeding history, anesthesia reactions, previous surgeries). Discuss all medications (prescription, over-the-counter, and herbal supplements) you are taking with your health care provider. Some medications need to be continued or stopped the day of surgery.
Depending on your procedure you may be ask to lose weight in order to help in your recover results.
Stop taking all non-steroidal anti-inflammatory medicines (Naprosyn, Advil, Motrin, Nuprin, Aleve, etc.) and blood thinners (Coumadin, Plavix, etc.) 1 to 2 weeks before surgery as directed by the doctor. Additionally, stop smoking, chewing tobacco, and drinking alcohol 1 week before and 2 weeks after surgery because these activities can cause bleeding problems. No food or drink is permitted past midnight the night before surgery.
Morning of surgery
- Shower using antibacterial soap. Dress in freshly washed, loose-fitting clothing.
- Wear flat-heeled shoes with closed backs.
- If you have instructions to take regular medication the morning of surgery, do so with small sips of water.
- Remove make-up, hairpins, contacts, body piercings, nail polish, etc.
- Leave all valuables and jewelry at home (including wedding bands).
- Bring a list of medications (prescriptions, over-the-counter, and herbal supplements) with dosages and the times of day usually taken.
- Bring a list of allergies to medication or foods.
Arrive at the hospital 2 hours before (surgery center 1 hour before) your scheduled surgery time to complete the necessary paperwork and pre-procedure work-ups. An anesthesiologist will talk with you and explain the effects of anesthesia and its risks. An intravenous (IV) line will be placed in your arm.
What happens during surgery?
Surgery takes approximately one hour
What happens after surgery?
You will awaken in the postoperative recovery area, called the PACU. Blood pressure, heart rate, and respiration will be monitored. Any pain will be addressed. Once awake, you will be moved to a regular room where you’ll increase your activity level (sitting in a chair, walking). Most patients can go home the same day, but depends on your response after surgery.
Discharge instructions
Discomfort
After surgery, pain is managed with narcotic medication. Because narcotic pain pills are addictive, they are used for a limited period (2 to 4 weeks). As their regular use can cause constipation, drink lots of water and eat high fiber foods. Laxatives (e.g., Dulcolax, Senokot, Milk of Magnesia) can be bought without a prescription. Thereafter, pain is managed with acetaminophen (e.g., Tylenol).
Restrictions
If you had a fusion, do not use non-steroidal anti-inflammatory drugs (NSAIDs) (e.g., aspirin; ibuprofen, Advil, Motrin, Nuprin; naproxen sodium, Aleve) for 6 months after surgery. NSAIDs may cause bleeding and interfere with bone healing.
Do not drive for 2 to 4 weeks after surgery or until discussed with your surgeon.
Avoid sitting for long periods of time.
Do not lift anything heavier than 10 pounds (e.g., gallon of milk). Do not bend or twist at the waist. Housework and yard-work are not permitted until the first follow-up office visit. This includes gardening, mowing, vacuuming, ironing, and loading/unloading the dishwasher, washer, or dryer.
Postpone sexual activity until your follow-up appointment unless your surgeon specifies otherwise.
Do not smoke. Smoking delays healing by increasing the risk of complications (e.g., infection) and inhibits the bones' ability to fuse.
Activity
You may need help with daily activities (e.g., dressing, bathing) for the first few days. Fatigue is common. Let pain be your guide.
Gradually return to your normal activities. Walking is encouraged; start with a short distance and gradually increase to 1 to 2 miles daily. A physical therapy program may be recommended.
Bathing/Incision Care
You may shower 1 to 4 days after surgery. Follow your surgeon’s specific instructions. No tub baths, hot tubs, or swimming pools until your health care provider says it’s safe to do so.
Staples or stitches, which remain in place when you go home, will need to be removed. Ask your surgeon or call the office to find out when.
When to Call Your Doctor
If your temperature exceeds 101° F, or if the incision begins to separate or show signs of infection, such as redness, swelling, pain, or drainage.
Recovery and prevention
Schedule a follow-up appointment with your surgeon for 1 weeks after discharge. Physical therapy may be necessary for some people.
The recovery time varies from 1 to 4 weeks depending on the underlying disease treated and your general health. You may feel pain at the site of the incision. The original pain may not be completely relieved immediately after surgery. Aim to keep a positive attitude and diligently perform your physical therapy exercises if prescribed.
Most people can return to work in 2 to 4 weeks or less with jobs that are not physically challenging. Others may need to wait at least 8 to 12 weeks to return to work for jobs that require heavy lifting or operating heavy machinery.
Recurrences of back pain are common. The key to avoiding recurrence is prevention:
- Proper lifting techniques
- Good posture during sitting, standing, moving, and sleepin
- Appropriate exercise program
- An ergonomic work area
- Healthy weight and lean body mass
- A positive attitude and relaxation techniques (e.g., stress management)
- No smoking
If you have any questions, please call us at 209-349-8428.

